What are FODMAPs?
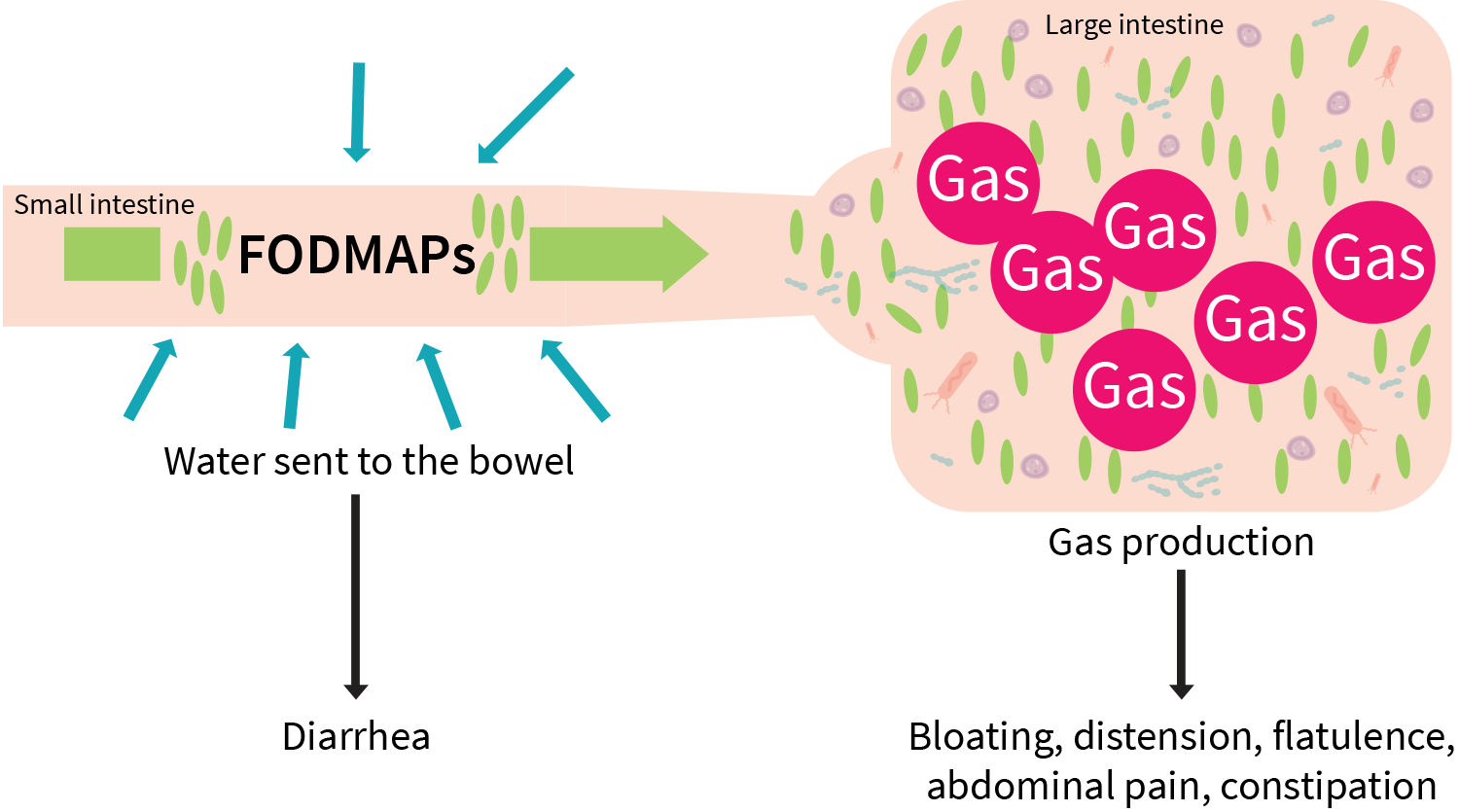
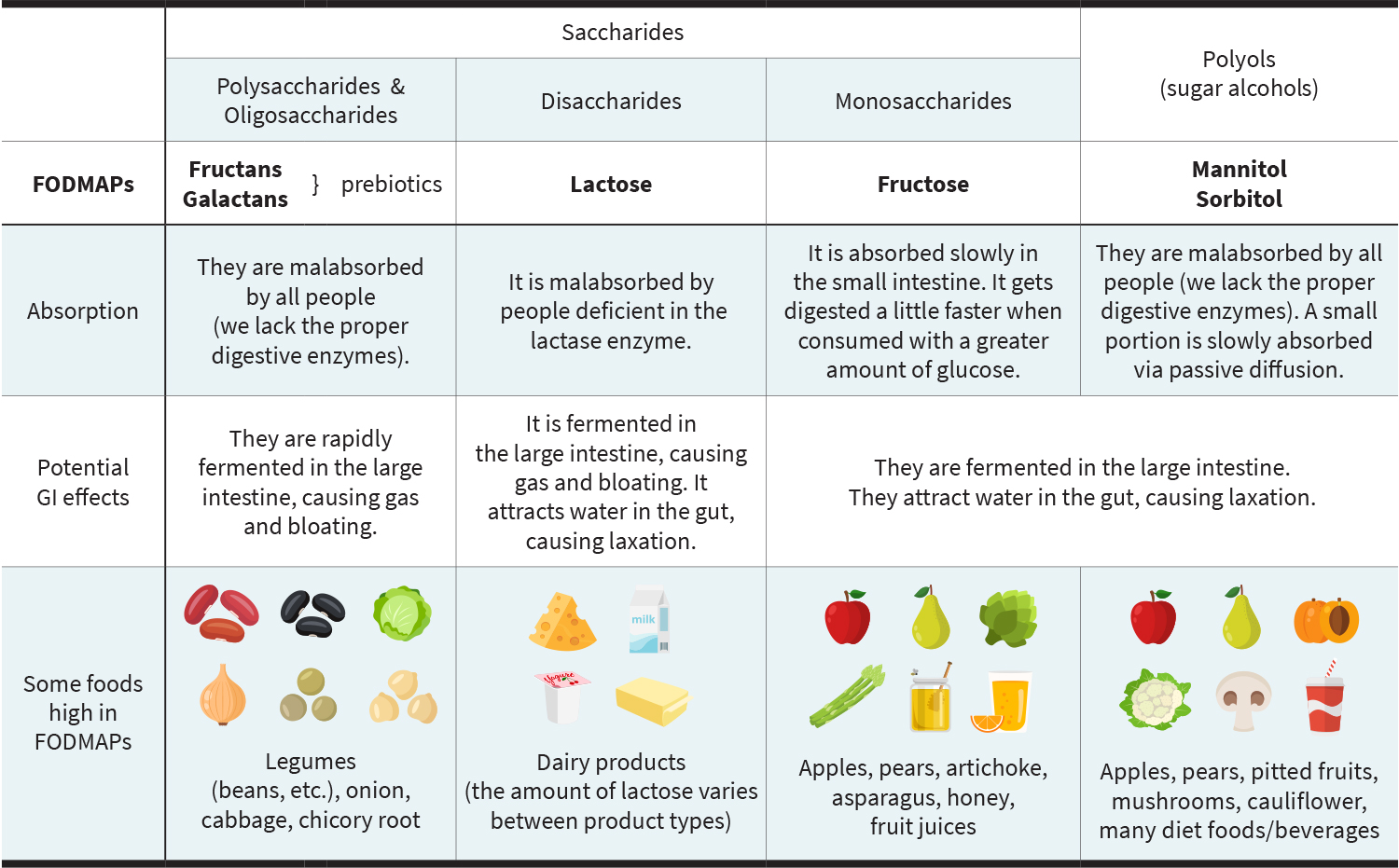
FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These are poorly absorbed, highly fermentable carbohydrates that can contribute to gas, bloating, and diarrhea due to their fermentability and attraction of water in the intestinal tract.
Click here to read more about specific FODMAPs and how they function in the intestines.
If you’re wondering about the differences between FODMAPs, fiber, and prebiotics, you’re not alone! Click here for a quick breakdown.
Which are low-FODMAP foods and which are high?
Many foods contain moderate to high concentrations of FODMAPs, with serving sizes dictating the overall FODMAP load. The way a food is prepared can also modify the FODMAP content. Meats and oils are almost always low-FODMAP foods. Fruits, vegetables, nuts, beans, grains, and many protein bars contain different types and amounts of FODMAPs, but some FODMAP categories are predominant in certain foods. Fructans are the main FODMAP found in wheat products, for example.
FODMAPs
Dietary FODMAP content can be confusing, so click here to read more about the most common sources and their low-FODMAP replacement options.
What is a low-FODMAP diet?
The low-FODMAP diet is thought to improve GI symptoms by reducing the content of FODMAPs in the intestines, resulting in lower intestinal water content and diminished gas production from microbial fermentation. It also modifies the gut microbiome, but the clinical significance of these changes is unknown. [1][2] Though it can be implemented in a variety of ways, the diet generally consists of an initial restriction phase, during which low-FODMAP foods replace those that are moderate or high, followed by a systematic reintroduction process to assess tolerance for each of the FODMAP groups. Dietary FODMAP sources are gradually elevated and diversified based on individual tolerance.
If you want to learn more about how to safely implement a low-FODMAP diet, click here.
Who is a good candidate for a low-FODMAP diet?
The low-FODMAP diet has been shown to improve quality of life as well as general IBS symptoms, including abdominal pain, bloating, diarrhea, and flatulence (though it is likely more effective for individuals with diarrhea-predominant IBS). [2][3] A short-term low-FODMAP diet may also reduce acute GI distress (commonly cramping and diarrhea) associated with intense endurance exercise. [4] Low-FODMAP formulas may also improve nutritional status in patients receiving enteral nutrition. [5] Additionally, in people with celiac disease, low-FODMAP, gluten-free diets are also associated with greater improvements in GI symptom scores compared with a gluten-free diet only.[6]
For reasons that are still unclear, people respond differently to a low-FODMAP diet, and some don’t see any improvements at all. Emerging research suggests that the fermentation capacity of a person’s microbiome might be one factor that explains—or could even predict—how well they’ll respond to a low-FODMAP diet. [7]
Click here to read more about the benefits of a low-FODMAP diet and how it compares to traditional dietary guidance for IBS.
Are there any risks associated with a low-FODMAP diet?
Long-term adherence to a low-FODMAP diet isn’t recommended, because it could be nutritionally inadequate and also appears to modify the microbiome in potentially unfavorable ways. [8][9] The low-FODMAP diet may pose a risk to people with inflammatory bowel disease (IBD), because they are already at risk of malnutrition.[10] The restrictive aspects of the low-FODMAP diet could also exacerbate an eating disorder. [11]
Click here to learn about the potential risks and limitations of a low-FODMAP diet.